All Providers
Main reasons for Improvement Notices
| Outcomes | Frequency (%) |
| Outcome 12: Requirements relating to workers |
35 |
| Outcome 8: Cleanliness and infection control |
35 |
| Outcome 16: Assessing and monitoring the quality of service provision |
30 |
| Outcome 7: Safeguarding people who use services from abuse |
25 |
| Outcome 9: Management of medicines |
20 |
| Outcome 10: Safety and suitability of premises |
14 |
| Outcome 1: Respecting and involving people who use services |
10 |
| Outcome 21: Records |
9 |
| Outcome 4: Care and welfare of people who use services |
7 |
| Outcome 14: Supporting workers |
6 |
| Outcome 11: Safety, availability and suitability of equipment |
3 |
| Outcome 2: Consent to care and treatment |
1 |
| Outcome 6: Cooperating with other providers |
1 |
| Outcome 17: Complaints |
1 |
| Outcome 13: Staffing |
0 |
| Outcome 5: Meeting nutritional needs |
0 |
__________________________________________________________________________________________________
CQC have recently reported that a number of providers have been contacted by people posing as CQC inspectors in an effort to gain access to services or information.
We recommend that before you speak to anyone:
- Ask the person for their details, e.g. Name, Region of Inspection team, ID number
- Do not give out any information and instead offer to call them back
- Call CQC on 03000 616161 to verify the details given to you.
All genuine CQC inspectors carry ID badges that include:
- a photograph of the inspector on the front
- a copy of a CQC warrant on the reverse
- the signature of our Chief Executive David Behan (older ID badges may have the signature of Cynthia Bower)
Note from the Editor:
Whislt all inspectors carry badges, it is difficult to check whether the ID is genuine or not as most of us don’t know what an original CQC ID badge looks like. So it is best to call CQC on 03000 616161 and check the inspector's details before you allow them onto your premises or give them any information.
If the CQC have concerns about your practice's compliance with the standards they will revisit. These type of inspection are carried out at any time in response to identified concerns e.g. patient complaints; serious failings or concerns higlighted in the initial visit.
Betweem April to 30 September 2014 CQC were trialling their new inspection model. The inspection reports that have been published based on these inspection have not got a star rating on any of the domains. Whilst we are not sure if CQC are going to update these reports, we have been advised by practices that they are being contacted by CQC in orfer to arrange a re-visit.
CQC are also scheduling re-visits based on their current Intelligent Monitoring publication where a practice has been indentified as having 'elevated risk' or 'risk' profile.
Editors Comment:
Our estimate is that a practice is spending anything from £1,000 to £7,000+ in time, effort and money just preparing for a CQC inspection and reinspection.
 |
If your organisation has been given a rating by the CQC, you are required to display the poster prominently in your main area and on your web site. Failure to do so will result in a fine and earn you a black mark against any future inspection. The guidance details the following points:
Want to see the full document? CLICK HERE to go to the CQC announcement. |
|---|
The City of London police have confirmed the arrest of a former Care Quality Commission (CQC) employee, on suspicion of bribery and money laundering, relating to allegations that care home proprietors have been offered better inspection reports in return for the payment of fees
Confirming that an inspector has been dismissed for gross misconduct, director of governance and legal services at the CQC, Louise Guss, said: “Having investigated allegations made to us about this inspector and found these were substantiated, we terminated their employment with immediate effect and referred the matter to the police.
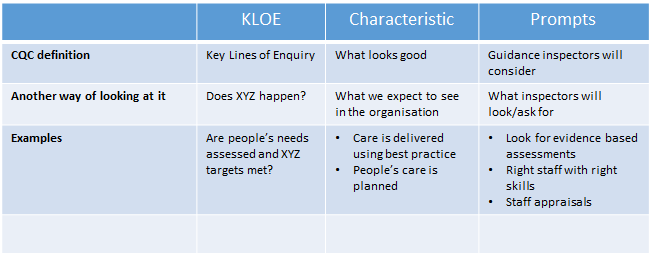
The acronym KLOE, stands for Key Lines of Enquiry.
The starting point for the inspection are the five key questions – are services safe, effective, caring, responsive and well-led?
A 'KLOE' is basically a set of 'key' questions the CQC will look at under each of five headings to reach a conclusion as to how your service should be rated.
Save
Save
Save
Save
Save
The CQC have outlined three types of inspections that wil be carried out. These are:
1. Comprehensive Inspections (Planned Inspections)
- How frequently you are inspected, the size of the inspection team and whether or not you get notice of inspection depends on the nature of the Service provision and organisation.
- The CQC call their new Inspection model under KLOEs a Comprehensive Inspection.
2. Focused Inspections (formerly known as follow-up inspections)
- To look at something that is of concern; usually after an improvement notice has been issued after a previous CQC visit.
- Focused inspections are carried out to check that compliance actions have been implemented
- These are smaller in scale than comprehensive inspections, although they follow a similar process.
- Generally a notice of the inspection will not be given (GP practices however still get notice of inspection)
3. Responsive Inspection
- These are carried out when concerns are raised over a provider’s compliance with the standards. (Information may come sources such as a whistle blower, the CCG, the GMC or a member of the public.)
The original aim was to inspect providers approximately once every 2 years, until every Provider had been inspected, then revise the interval depending on their rating.
This has not worked out, and there are still hundreds of Providers who have not seen a visit from as far back as 2015.
The regime has become fragmented, with GPs slated to get a visit every 5 years if they have a good rating, but not all other providers are included in this new scheme.
The focus of CQC inspections is the experiences people have when they receive care and the impact the care has on their health and wellbeing. CQC make their judgements against the regulations, and the judgements they make are informed by these experiences. This is why inspectors spend a lot of their time on an inspection talking to patients, their families and their carers. They’ll check their findings in a number of ways, for example by looking at records or speaking with staff, to reach their judgements.
"We won’t normally spend a great deal of time reading policy or procedure documents, unless we need to look at them to substantiate other evidence or what staff or patients have told us about their experiences."
Registered providers or managers have five working days to make written representations about a warning notice issued to them.
They also have 10 working days to challenge the factual accuracy of the report which led to the CQC's judgement to issue a warning notice.
These two processes run parallel with each other.
If the representations are not upheld, the CQC will make public the fact that a warning notice has been issued to an organisation.release and in the relevant review of compliance report.
For a copy of the Warning Notice Representations form Click Here.
The CQC will normally brief the local, national and trade media when they:
- Publish review of compliance reports where they have judged non compliance has a major impact on people.
- Publish review of compliance reports that follow up compliance conditions set during initial registration.
- Take enforcement action against a provider.
How do CQC gather the Information
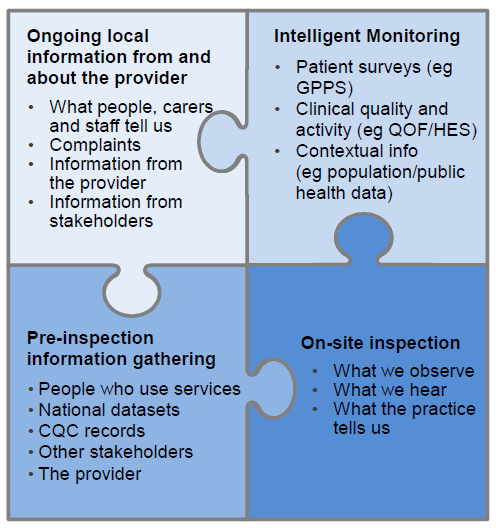 |
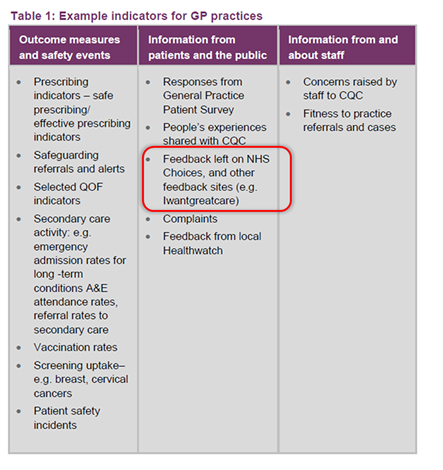
This graphic shows where the CQC will get information about you. Most of it is obvious: Complaints to CQC; whistle-blowers; Your registration form; IG Toolkit; QOF reports; Patient surveys etc. A basic rule of thumb is that if you have published information about yourself to the NHS, they will use that in the pre-preparation. In addition, if anyone else has posted information about you, they will also use that under the header “People who use services” The data in the IM report includes information from:
Whilst most of this is expected, it is worrying that in addition to NHS Choices the CQC believe that information from private websites will also be considered legitimate “intelligence” for an inspection. CQC promoting a private website in its guidelines is quite extraordinary we think! This data gathering angle has the potential for a worrying trend.
CQC will also ask local organisations to provide information, including: Some local organisations have a responsibility to gather and use people’s experiences of care and we will request information they hold, for example: CQC will publish further detail about the information we will request, but it is likely to include: |
 |
Save
Save
Save
Save
Save
Save
Save
Save
Save
Save
Save
Save
In simplified terms, the regulations require that you must ensure that the condition of your premises and equipment meet infection control standards.
Neither the CQC nor Infection Control regulations specify what surfaces and fixtures should be selected because this will vary enormously depending on the type of service you provide.
What this means is that the decision on what is suitable is entirely up to you as long as you ensure that everything is as clean and infection free as is reasonably possible.
When you choose surfaces, fixtures, fittings, furniture and equipment, you have to use common sense and best practice to ensure that the products are designed or selected bearing in mind easy cleaning, compliance with infection control criteria and durability in a healthcare environment.
Rule of thumb
In most cases, when you choose products or are deciding whether to change, your choice of equipment usually boils down to a balance between whether to get something that is more efficient/practical to keep clean, usually more expensive, or something that will still do the job but requires more maintenance. Either is acceptable as long as long as it is kept infection free.
Flooring
There is no specific legislation that says you MUST have flooring with coved skirting. However, it is best practice and reduces contamination from ledges/mouldings and gaps under skirting boards. Most importantly it is a lot easier to keep clean and infection free.
Carpets
There is no legislation that forces you to replace your carpets in favour of hard flooring or lino. You can have carpets as long as you keep them clean and infection free. Hard flooring and lino are however much easier to keep clean, especially when you have spills and high traffic of patients walking in with dirty shoes. The choice is entirely yours depending on where the carpets are installed, and whether you are prepared to spend more time and money cleaning carpets when it is so much easier to maintain hard floors.
Toys
All toys in regular use need to be cleaned daily.
Soft toys (porous or fabric) are hard to disinfect and tend to rapidly become re-contaminated after cleaning. They are generally considered a high infectious risk and unsuitable for doctors' waiting rooms.
Soft toys are not recommended unless they are laundered daily at temperatures to achieve thermal disinfection.
Taps
Best Practice says that taps should enable the user to turn them off without contaminating hands; also that swan neck taps should be avoided as they do not empty fully after use. (Legionella)
You do not have to change your taps as long as you can assess and manage the risk of contamination when using traditional mixer taps. The decision is simple; you need to clean ordinary taps more often than hands free taps, and your choice is a balance between the cost of purchase, cost of maintenance, and cleaning effort over the long term.
Sinks
The guidance states that sinks should be large enough and with curved sides to contain and reduce splashes and allows staff to perform accepted hand hygiene techniques.
The Guidelines have no legal status and are not enforceable.
The CQC Regulations and the CQC Guidance are two completely separate things.
The Regulations are the legal requirements as set out in the Health and Social Care Act 2008 (Regulated Activities) Regulations 2010. This is what you must follow.
The Guidelines, which contain the "28 Outcomes", are commonly mistaken for the regulations itself. These guidelines are exactly what the title says, just guidelines issued by the CQC to help you along as to the sort of issues you should be looking at to achieve compliance.
This is stated very clearly in the Guidelines right at the beginning on page 9 :
The legal status of the guidance for providers:
"Although we must take it into account when making decisions about a provider’s compliance with the regulations and in tribunals and courts, the guidance is not enforceable in its own right."
Healthcare Providers
CQC has widely missed original targets
When CQC started, they aimed to inspected every GP by 2016, we predicted that they wouldn't meet the target, and based on initial performance it would have taken 14 years to achieve that.
By 2016, many more inspectors had been recruited, and the rules and guidelines have changed beyond recognition.
Where are we now?
The CQC web site is not the easiest to follow if you are looking for the numbers. Approximately 18% of practices have still not been inspected and we can expect all sites to be inspected at least once by sometime in 2018. We originally estimated they would achieve this by August 2017.
Editor's Note:
A common comment we hear from practices already visited is "there is no need to be so dilligent anymore as we've already had our inspection". A similar effect is observed with traffic cameras,where everyone slows down just enough to not get caught, and speeds as soon as they pass the danger.
The CQC is now advocating no visits for 5 years if a practice demonstrates good behaviour but with random unannounced visits.
Just to remind oursleves, the original aim was "To inspect a primary medical service provider approximately once every 2 years, but some practices may be inspected more often".
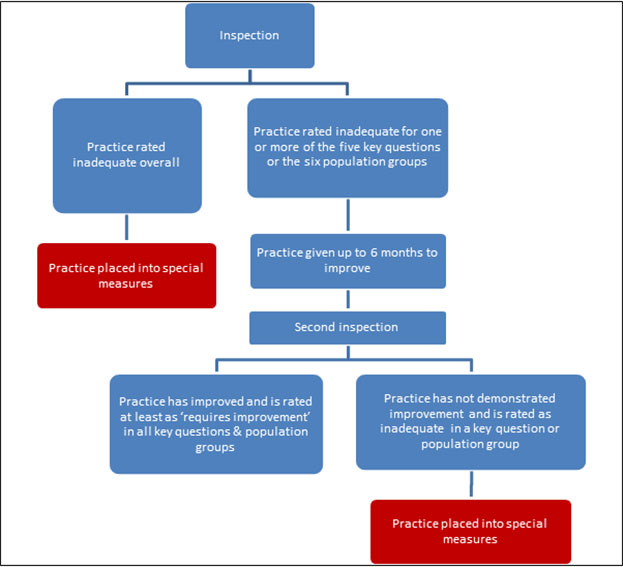
What are Special Measures?
Special measures came into effect from April 2015.
The purpose of these 'measures' by CQC is to ensure that practices that are found to be inadequate are not allowed to carry on unless they fix the problem. So how does this work?
- Practices will be given a fixed time for improvement and will be re-inspected within the following 6 months. If there is insufficient improvement, the practice will be put into special measures.
- If however the CQC think that the problems are significant enough to cause risk to patients, or the provider will not be able to sort them out themselves, they will be put into special measures straight away.
- After this, the provider will have a maximum of 6 months to fix the problems, else proceedings will commence to cancel their licence to trade.
A provider can be put into special measures AND also be subject to other enforcement action at the same time.
Save
Save
Save
Save
Save
Save
Save
Save
Free money - a £5,000 grant
This grant is only available to GP practices, all other providers have to self-finance their compliance issues.
For practices that are put under special measures, NHS England and the RCGP have agreed a £5,000 grant and a 68 page framework to help GP Practices to get back on their feet, but there are some conditions attached.
- You don’t get the cash, the RCGP gets it, and you have to match this with your own £5,000, so the RCGP get £10,000 in total. Still, you are getting £10,000 worth of services for half price.
- The RCGP has its own conditions attached to this, and here is a quick summary
- All payments to the RCGP are up front
- If you get other independent support on top, these consultants “must” liaise with the RCGP
- There are no warranties or guarantees
- You cannot get a refund if you feel the project was ineffective
The contract is a fixed fee contract but can be terminated by the RCGP on various grounds.
A refund may be made for unused time, although it is unclear how a fixed price contract will then be adjusted on a time charge methodology.
There no indication in the contract of staff seniority and hourly rates.
Compared to Legal and Consultancy firms:-
Legal firms are bound by regulations to full disclosure of expected charges, and have to keep you informed of changes throughout the assignment. In addition, you are protected by a dispute procedure; a regulatory body; and an ombudsman to whom you can take your compliant to. If the firm proves incompetent, you have contractual and legal remedies for independent costing, refund and damages.
Helpful chart published by the CQC
Save
Save
Save
Save
Save
Save
Save
From April 2014 GP practices will be given two weeks’ notice before a CQC inspection under major changes to the way visits are carried out.
A CQC statement has said: ‘CCGs are being given at least four weeks advance notice that their area has been selected and GP practices in those areas will have at least two weeks’ notice of an inspection as opposed to the previous 48 hours, CQC reserve the right however to inspect unannounced at any time where a practice is identified as a risk.
As reported by Pulse, the Chief inspector of primary care Professor Steve Field has claimed that the change heralds a ‘new approach’ in the way the CQC works with GP practices, aiming to support them to raise standards.
In 2012 a concession had been agreed and only GP practices were given a 48 hours’ notice.
Under major changes to the way visits are carried out, from April 2014 this 48 hour period increased to a two weeks’ notice before a CQC inspection.
A CQC statement has said: ‘CCGs are being given at least four weeks advance notice that their area has been selected and GP practices in those areas will have at least two weeks’ notice of an inspection as opposed to the previous 48 hours, CQC reserve the right however to inspect unannounced at any time where a practice is identified as a risk.
As reported by Pulse, the Chief inspector of primary care Professor Steve Field has claimed that the change heralds a ‘new approach’ in the way the CQC works with GP practices, aiming to support them to raise standards.
Whilst a 2 week notice period is the CQC's 'official' position, find out more as to what happens in reality.
For cleaning utilities like the slop hopper, there is no specific legislation that says you must have this. However, it is good practice, and avoids cleaners from using kitchen and toilet sinks as substitutes. In short, you do not have to have a slop hopper, but whatever you use, you should follow the following principles:-
- Your main port of call is to make sure the cleaning methodology follows infection control guidelines at all times
- Usage and installation must ensure there is no risk of cross-contamination
- The best person to advise you is the manufacturer as they will be the “ultimate experts”
Most organisations that have a slop hopper, usually have a designated janitorial area, separate from kitchen, clinical and public facilities. This is quite difficult in older GP premises and they often install these in a staff toilet area, which is not ideal as cross contamination risk is still high.
When in doubt about any equipment, the safest option is to speak to the manufacturer and use a recommended/qualified installer, simply because they understand better than all others exactly how/where to install as they do this on a daily basis.