The leading independent resource for CQC compliance
 |
|
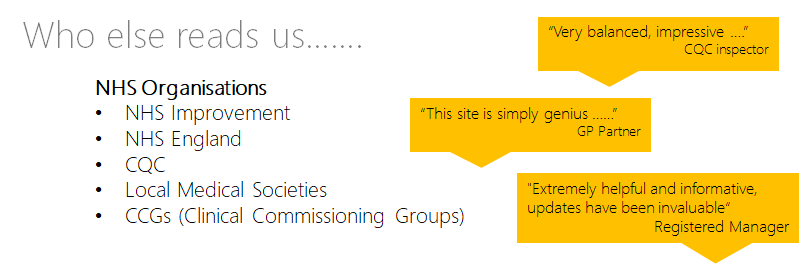
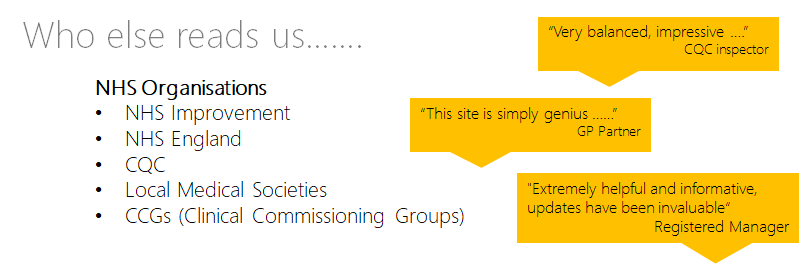
| If you are part of an NHS body or a Membership or Regulatory organisation, you may qualify to use our products as a Reference Standard. |
 |
|
| If you are part of an NHS body or a Membership or Regulatory organisation, you may qualify to use our products as a Reference Standard. |